Consider this: Right now, as you’re sitting there, there’s a battle raging in your belly. Some 1,000 species of bacteria are duking it out, trying to establish dominance. Why should you care? Because whether the good bacteria in your gut or the bad triumph doesn’t just decide how well you digest your dinner, respond to allergens and fend off diseases—it also helps determine how much weight you’re likely to gain. Or lose.
“Simply put, if you get the microbiome—that collection of bacteria inside you—healthy, you will lose weight,” says Raphael Kellman, MD, a New York City physician and author of The Microbiome Diet. “It’s less about eating a certain percentage of carbohydrates, protein and fat than about correcting the overgrowth of unhealthy bacteria, which is making you crave the wrong foods, triggering inflammation.”
What exactly is “the gut”?
Our gut is home to approximately 100,000,000,000,000 (100 trillion) microorganisms. That’s such a big number our human brains can’t really comprehend it. One trillion dollar bills laid end-to-end would stretch from the earth to the sun – and back – with a lot of miles to spare. Do that 100 times and you start to get at least a vague idea of how much 100 trillion is.
 The human gut contains 10 times more bacteria than all the human cells in the entire body, with over 400 known diverse bacterial species. In fact, you could say that we’re more bacterial than we are human. Think about that one for a minute.
The human gut contains 10 times more bacteria than all the human cells in the entire body, with over 400 known diverse bacterial species. In fact, you could say that we’re more bacterial than we are human. Think about that one for a minute.
We’ve only recently begun to understand the extent of the gut flora’s role in human health and disease. Among other things, the gut flora promotes normal gastrointestinal function, provides protection from infection, regulates metabolism and comprises more than 75% of our immune system. Dysregulated gut flora has been linked to diseases ranging from autism and depression to autoimmune conditions like Hashimoto’s, inflammatory bowel disease and type 1 diabetes.
Recent research has shown that the gut flora, and the health of the gut in general, also play a significant role in both obesity and diabetes. I’ve seen this anecdotally in my practice as well. Nearly every patient I treat with a blood sugar issue also has a leaky gut, a gut infection, or some other chronic inflammatory gut condition.
We now know that the composition of the organisms living in your gut determines – to some extent, at least – how your body stores the food you eat, how easy (or hard) it is for you to lose weight, and how well your metabolism functions. Let’s take a closer look at the mechanisms involved.
Intestinal bacteria drive obesity and metabolic disease
A study published this year in Science magazine found that mice without a protein known as toll-like receptor 5 (TLR5) in their gut gain excessive weight and develop full-blown diabetes and fatty liver disease when fed a high-fat diet. If we think of the gut flora as a community, TLR5 is like a neighborhood police force that can keep the houligans in check. Without TLR5, bad bacteria can get out of control.
The study authors found that these bad bacteria caused a low-grade inflammation in the mice, which caused them to eat more and develop insulin resistance. They also found that treating these mice with strong antibiotics (enough to kill most of the bacteria in the gut) reduced their metabolic abnormalities.
But the most interesting part of this study is what happened when the researchers transferred the gut flora from the TLR5-deficient overweight mice into the guts of skinny mice: the skinny mice immediately started eating more and eventually developed the same metabolic abnormalities the overweight mice had. In other words, obesity and diabetes were “transferred” from one group of mice to the other simply by changing their gut flora (as shown in the image below).
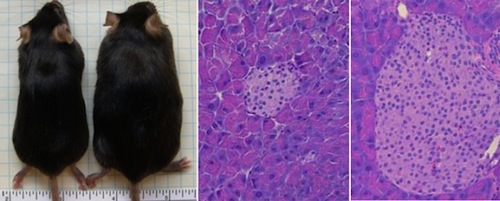
In the study on TLR5 deficient mice mentioned above, the mice with too much bad bacteria in their guts experienced an increase in appetite and ate about 10 percent more food than their regular relatives. But it wasn’t just that these mice were hungrier and eating more; their metabolisms were damaged. When their food was restricted, they lost weight – but still had insulin resistance.
Other studies have shown that the composition of the gut flora differs in people who are obese and diabetic, and people who are normal weight with no metabolic irregularities.
One possible mechanism for how changes in the gut flora cause diabesity is that different species of bacteria seem to have different effects on appetite and metabolism.
A flurry of ground-breaking findings are helping to connect the dots about how our gut bacteria may shape our, well, shape. In a study in the British Journal of Nutrition, obese women who took a probiotic supplement (of the bacteria Lactobacillus rhamnosus) lost twice as much weight and fat over about six months—and were better at keeping it off—as those who took a placebo. Probiotics may have helped by controlling the women’s appetites, which seem to have waned as their microbiomes changed.
Unhealthy gut bacteria also produce food cravings: A study published in BioEssays suggests that some microbes may drive us to eat doughnuts or another tempting treat. These gut bugs send chemical messages to the brain that sway our appetite and mood—perhaps making us feel anxious until we gobble a square of dark chocolate or a T-bone steak.
Other studies have shown that changes in the gut flora can increase the rate at which we absorb fatty acids and carbohydrates, and increase the storage of calories as fat. This means that someone with bad gut flora could eat the same amount of food as someone with a healthy gut, but extract more calories from it and gain more weight.
Bad bugs in the gut can even directly contribute to the metabolic syndrome by increasing the production of insulin (leading to insulin resistance), and by causing inflammation of the hypothalamus (leading to leptin resistance).
Modern life: screws up our gut and makes us fat and diabetic
What all of this research suggests is that healthy gut bacteria is crucial to maintaining normal weight and metabolism. Unfortunately, several features of the modern lifestyle directly contribute to unhealthy gut flora:
– Antibiotics and other medications like birth control and NSAIDs
– Diets high in refined carbohydrates, sugar and processed foods
– Diets low in fermentable fibers
– Dietary toxins like wheat and industrial seed oils that cause leaky gut
– Chronic stress
– Chronic infections
We also know that infants that aren’t breast-fed and are born to mothers with bad gut flora are more likely to develop unhealthy gut bacteria, and that these early differences in gut flora may predict overweight and obesity in the future.
It’s interesting to note that the diabesity epidemic has neatly coincided with the increasing prevalence of factors that disrupt the gut flora. I’m not suggesting that poor gut health is the single cause of obesity and diabetes, but I am suggesting that it likely plays a much larger role than most people think.
How is Your Gut?
Despite whether or not you already eat relatively healthy, your gut may still be a little out of whack. Here’s how to check:
Gut check #1: Get Your Two P’s
Basically, it all begins with probiotics and prebiotics, components of food believed to play an important role in improving gut health. Probiotics are a type of good bacteria, similar to the ones that already reside in your gut. Ingesting these organisms aids digestion and helps change and repopulate intestinal bacteria to balance what doctors refer to as “gut flora.” Prebiotics are plant-fiber compounds, also found in food, that pass undigested through the upper part of the gastrointestinal tract and help stimulate the growth of good bacteria. When pre- and probiotics are combined, they become an intestinal power couple (or, in blunter terms, they kick nutritional butt).
Gut check #2: Go Live
Fermented foods deliver probiotics directly to the gut. A cup of yogurt a day? It’s a nice start. Look for products that say “live and active cultures” on the label, and be careful when it comes to fruit-infused flavors: Some are loaded with sugar, which can feed bad bugs, so be sure to check the ingredients and aim for fewer than 15 grams per serving. For even more probiotics, try Greek yogurt or kefir, a tangy dairy drink that’s packed with good bugs. A 2011 Harvard study found that yogurt was more strongly linked to weight loss than any other health food. In fact, people who ate an extra serving a day lost nearly a pound every four years.
Gut check #3: Down Some Fiber
It does more than fill you up: Research shows that foods that are high in fiber help promote the growth of friendly bacteria. Case in point: In a University of Illinois study, people who ate high-fiber snack bars experienced a growth of anti-inflammatory bacteria in their bellies.
Gut check #4: Mix Up Your Menu
Eat an assortment of foods to encourage a more varied metropolis in your belly. Recent studies suggest that the intestines of lean people look more like bustling cities than sleepy towns. (Translation: They’re densely populated and diverse.) One study showed that individuals who had a healthy weight, body mass index, waist circumference and blood sugar level were more apt to have high levels of three different types of bacteria—Firmicutes, Bifidobacteria and Clostridium leptum. What’s more, in a pair of French studies, people with diverse gut microbiomes were less likely to be obese or at risk of diabetes. Plus, their intestinal ecosystems were home to fewer pro-inflammatory bacteria. It’s easy to change up your meals: If you had salad with grilled chicken yesterday, for example, go with a fish taco or a tofu stir-fry today.
Gut check #5: Skip Bad-News Foods
What you don’t eat is every bit as crucial as what you do add to your diet. Keep your gut flora fit by cutting back on these offenders.
Refined carbs
Fatty and sugary foods not only tend to lack fiber—which is ideal food for the microbiome—but can also cause bad bacteria to thrive. And let’s face it: If you’re pounding that bag of potato chips, chances are you’re not munching on celery sticks, blueberries and other gut-friendly eats.
Animal protein
A diet heavy in fat and protein (such as meat and cheese) feeds a type of bacteria, Bilophilia, that has been linked to inflammation. Lawrence David, PhD, assistant professor at Duke University’s Institute for Genome Sciences and Policy, saw the levels of this bacteria shoot up in study participants scarfing ribs and brisket, but not in those eating squash and lentils. Dr. Kellman suggests limiting red meat to once a week. It’s smart for your heart—and hips!
How to maintain and restore healthy gut flora
The most obvious first step in maintaining a healthy gut is to avoid all of the things I listed above. But of course that’s not always possible, especially in the case of chronic stress and infections, and whether we were breast-fed or our mothers had healthy guts.
If you’ve been exposed to some of these factors, there are still steps you can take to restore your gut flora:
- Remove all food toxins from your diet
- Eat plenty of fermentable fibers (starches like sweet potato, yam, yucca, etc.)
- Take a high-quality probiotic, or consider more radical methods of restoring healthy gut flora
- Treat any intestinal pathogens (such as parasites) that may be present
- Take steps to manage your stress
Fortunately, we can begin to take control by feeding our microbiome the right foods. “I tell my patients, ‘The bacteria follow the food,’” says gastroenterologist Robynne Chutkan, MD, founder of the Digestive Center for Women in Chevy Chase, Md., and author of Gutbliss.“What we eat dictates the kind of bacteria we grow in our gut garden.”
This is big news: There are trillions of microbes in your belly that will—if you feed them well—help you fight flab and win.
Sources:
http://www.health.com/health/article/0,,20859953,00.html
https://chriskresser.com/a-healthy-gut-is-the-hidden-key-to-weight-loss/